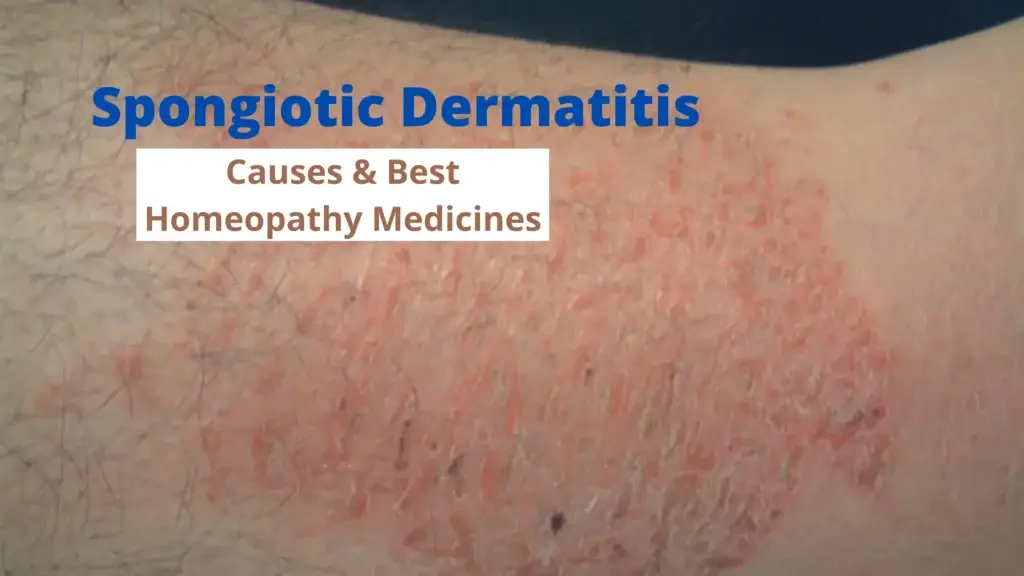
Spongiotic dermatitis, a term that often appears in dermatology reports, refers to a specific pattern of skin inflammation characterized by fluid accumulation between the cells of the epidermis. This condition can manifest in various forms, presenting a wide range of symptoms that can significantly impact a person’s quality of life. Understanding spongiotic dermatitis is crucial for effective management and treatment, as it encompasses a variety of underlying causes, including allergic reactions, irritant dermatitis, and more complex immunological conditions.
In this blog, we will delve into the intricacies of spongiotic dermatitis, exploring its symptoms, causes, and the latest treatment options available. We aim to provide a comprehensive guide that not only educates but also empowers individuals dealing with this condition. Whether you are a patient, a caregiver, or simply someone interested in dermatological health, this article will offer valuable insights into managing spongiotic dermatitis effectively. Join us as we uncover the complexities of this skin condition and learn how to navigate its challenges with informed confidence.
What is Spongiotic Dermatitis
Spongiotic dermatitis is a form of eczema characterized by a distinct pattern of skin inflammation visible under a microscope. The term “spongiosis” refers to the presence of intercellular edema in the epidermis, which means there is an accumulation of fluid between the skin cells. This fluid buildup causes the skin cells to appear separated or “spongy,” hence the name.
Spongiotic Dermatitis Types
Spongiotic dermatitis can be classified into several types based on the underlying cause and clinical presentation. Here are the main types:
Allergic Contact Dermatitis
Allergic contact dermatitis occurs when the skin comes into contact with an allergen, triggering an immune response. Common allergens include certain metals (like nickel), fragrances, preservatives, and plants like poison ivy. Symptoms can range from mild redness and itching to severe blistering and swelling.
Irritant Contact Dermatitis
Irritant contact dermatitis is caused by direct damage to the skin from a substance, such as harsh chemicals, detergents, or prolonged exposure to water. Unlike allergic contact dermatitis, it doesn’t involve an immune response but results from the irritating effects of the substance on the skin. This type often affects the hands and areas frequently exposed to irritants.
Atopic Dermatitis
Atopic dermatitis, also known as eczema, is a chronic condition that often begins in childhood and can persist into adulthood. It’s characterized by dry, itchy, and inflamed skin, and is commonly associated with other atopic conditions like asthma and hay fever. The exact cause is unknown, but it involves genetic factors and an overactive immune response.
Nummular Dermatitis
Nummular dermatitis presents as round, coin-shaped patches of inflamed skin that are often itchy and may ooze or become crusty. This type can be triggered by dry skin, environmental factors, or skin injuries. It’s more common in adults and can be challenging to treat due to its chronic nature.
Dyshidrotic Eczema
Dyshidrotic eczema, also known as pompholyx, involves the development of small, deep-seated blisters on the palms, fingers, and soles of the feet. These blisters are often intensely itchy and can be triggered by stress, allergies, or exposure to certain metals. The exact cause is unknown, but it can be recurrent and difficult to manage.
Seborrheic Dermatitis
Seborrheic dermatitis affects areas of the skin rich in sebaceous glands, such as the scalp, face, and upper chest. It manifests as red, scaly, and greasy patches, often with dandruff. This type is associated with an overgrowth of a yeast called Malassezia and can be influenced by genetic, environmental, and hormonal factors.
Stasis Dermatitis
Stasis dermatitis occurs in individuals with poor circulation, typically in the lower legs. It’s often associated with chronic venous insufficiency, where blood pools in the veins, leading to swelling, redness, and eventually skin changes. This type can cause significant discomfort and lead to ulcers if not managed properly.
Spongiotic Dermatitis Causes
Spongiotic dermatitis can be triggered by a variety of factors, often related to the body’s immune response. Common causes include:
Allergic Reactions
Exposure to allergens such as pollen, pet dander, certain foods, or insect bites can lead to an overactive immune response, causing inflammation and spongiosis.
Irritants
Contact with harsh chemicals, soaps, detergents, or other skin irritants can damage the skin’s protective barrier, leading to dermatitis.
Genetic Predisposition
A family history of eczema, asthma, or allergies can increase the likelihood of developing spongiotic dermatitis.
Environmental Factors
Changes in weather, humidity, and exposure to environmental pollutants can trigger flare-ups.
Stress
Emotional stress can exacerbate skin conditions by weakening the immune system, making the skin more susceptible to inflammation.
Infections
Bacterial, viral, or fungal infections can cause or worsen dermatitis by disrupting the skin’s natural balance.
Autoimmune Disorders
Conditions such as psoriasis or lupus, where the immune system attacks healthy skin cells, can also result in spongiotic dermatitis.
Spongiotic Dermatitis Symptoms
Spongiotic dermatitis manifests through various symptoms, which can range from mild to severe and may affect different parts of the body. Common symptoms include:
Itching
One of the most prevalent symptoms, itching can vary from mild to intense, often leading to scratching and further skin irritation.
Redness
Inflamed, red patches of skin are a typical sign of spongiotic dermatitis, indicating underlying inflammation and irritation.
Swelling
Affected areas may swell due to fluid accumulation in the skin, contributing to discomfort and pain.
Blisters
In more severe cases, small, fluid-filled blisters may appear, which can burst and lead to crusting and scabbing.
Dry, Flaky Skin
The skin may become dry, flaky, and scaly, often peeling off and creating a rough texture.
Rash
A general rash may develop, spreading over large areas of the body or remaining localized.
Pain or Discomfort
Due to the combination of itching, swelling, and blisters, patients may experience significant pain or discomfort.
Thickened Skin
Chronic cases of spongiotic dermatitis can lead to lichenification, where the skin becomes thickened and leathery from prolonged scratching and rubbing.
Cracks or Fissures
Severely dry and inflamed skin can crack, leading to painful fissures that may bleed and increase the risk of infection.
Risk Factors for Spongiotic Dermatitis
Several risk factors can increase the likelihood of developing spongiotic dermatitis. These include:
Genetic Predisposition
A family history of dermatitis, eczema, or other allergic conditions can increase the risk, suggesting a genetic component to the disease.
Allergies
Individuals with a history of allergies, such as hay fever, asthma, or food allergies, are more prone to developing spongiotic dermatitis due to their heightened immune responses.
Environmental Factors
Exposure to certain environmental triggers like pollutants, harsh chemicals, or allergens can exacerbate or trigger the condition. Common irritants include soaps, detergents, and synthetic fabrics.
Stress
High levels of stress can weaken the immune system and worsen symptoms of spongiotic dermatitis. Stress management techniques can be beneficial in mitigating this risk factor.
Immune System Dysfunction
Conditions that affect the immune system, such as autoimmune diseases, can increase susceptibility to spongiotic dermatitis. An overactive immune response can lead to the inflammation characteristic of this condition.
Age
Spongiotic dermatitis can affect individuals of any age but is more common in infants and young children. However, it can also persist or develop in adulthood.
Skin Barrier Defects
Deficiencies in the skin’s barrier function, often due to a lack of natural oils or other protective components, can make the skin more vulnerable to irritants and allergens.
Occupational Exposure
Jobs that involve frequent exposure to irritants, such as healthcare, cleaning, or hairstyling, can increase the risk of developing spongiotic dermatitis due to constant contact with potential triggers.
Climate
Living in regions with extreme weather conditions, either very dry or very humid climates, can aggravate the skin and contribute to the development of spongiotic dermatitis.
Hygiene Practices
Excessive washing or bathing, especially with hot water or harsh soaps, can strip the skin of its natural oils, leading to dryness and increased susceptibility to dermatitis.
Infections
Certain bacterial or viral infections can act as triggers for spongiotic dermatitis, particularly in individuals with compromised immune systems or pre-existing skin conditions.
Diagnosis of Spongiotic Dermatitis
Diagnosing spongiotic dermatitis involves a combination of clinical evaluation, patient history, and diagnostic tests. Here are the key steps:
Clinical Examination
Diagnosing spongiotic dermatitis begins with a thorough clinical examination by a dermatologist. The doctor will inspect the affected skin areas, looking for typical signs such as redness, swelling, and blisters. They may also inquire about the patient’s medical history, recent exposures to allergens or irritants, and any medications being used.
Skin Biopsy
A definitive diagnosis often involves a skin biopsy, where a small sample of affected skin is taken for microscopic examination. This helps confirm the presence of spongiotic changes in the skin layers, characterized by intercellular edema (fluid buildup) and inflammatory infiltrates.
Patch Testing
In cases suspected of being triggered by allergens or contact irritants, patch testing may be conducted. This involves applying small amounts of potential allergens or irritants to the skin under adhesive patches for a period of time. Reactions are monitored to identify specific triggers contributing to the dermatitis.
Differential Diagnosis
Distinguishing spongiotic dermatitis from other skin conditions with similar symptoms, such as allergic contact dermatitis, psoriasis, or fungal infections, is crucial. This involves considering the clinical presentation, medical history, and sometimes additional diagnostic tests to rule out other potential causes.
Laboratory Tests
In some cases, blood tests or other laboratory investigations may be recommended to assess for underlying conditions or systemic involvement contributing to dermatitis symptoms.
Follow-up and Monitoring
After diagnosis, ongoing monitoring and follow-up appointments with a dermatologist are essential. This ensures proper management of symptoms, identification of triggers, and adjustment of treatment plans as needed to achieve optimal skin health and quality of life for the patient.
Spongiotic Dermatitis Management
Spongiotic dermatitis management typically involves a multifaceted approach aimed at alleviating symptoms, reducing inflammation, preventing flare-ups, and promoting skin healing. Treatment options often include:
1. Topical Treatments:
Topical corticosteroids are commonly prescribed to reduce inflammation and itching. Non-steroidal options like calcineurin inhibitors may also be used, particularly on sensitive skin areas or for long-term management.
2. Emollients and Moisturizers:
Regular application of moisturizers and emollients helps maintain skin hydration, strengthen the skin barrier, and reduce dryness. This is crucial in managing symptoms and preventing exacerbations.
3. Avoiding Triggers:
Identifying and avoiding triggers such as allergens, irritants, certain fabrics, and extremes of temperature can help minimize flare-ups and manage symptoms effectively.
4. Oral Medications:
In severe cases or when topical treatments are insufficient, oral corticosteroids or oral antihistamines may be prescribed to control inflammation and itching.
5. Phototherapy:
Phototherapy, using ultraviolet (UV) light, can be beneficial in some cases, particularly when topical treatments and other medications are not effective.
6. Lifestyle Modifications:
Adopting gentle skin care practices, including using mild soaps and avoiding prolonged bathing in hot water, can help maintain skin health and reduce irritation.
7. Stress Management:
Stress can exacerbate symptoms of spongiotic dermatitis. Techniques such as meditation, yoga, or counseling may be helpful in managing stress levels.
8. Regular Follow-up:
Regular follow-up visits with a dermatologist are essential to monitor progress, adjust treatment plans as needed, and prevent complications associated with chronic dermatitis.
Homeopathic Medicine for Spongiotic Dermatitis
Unlock the natural and holistic potential of homeopathy in treating diseases and bodily disorders. Here, we explore a range of homeopathic medicines known for their effectiveness. The 10 best homeopathic medicine for Spongiotic Dermatitis are as follows –
- Graphites
- Sulphur
- Rhus Toxicodendron
- Arsenicum Album
- Mezereum
- Petroleum
- Calendula Officinalis
- Hepar Sulphuris Calcareum
- Antimonium Crudum
- Natrum Muriaticum
Graphites
Overview:
Graphites is beneficial for spongiotic dermatitis where the skin is dry, rough, and cracked. It helps in cases where there is oozing of sticky discharge from eruptions, which may be moist and exuding a honey-like fluid.
Key Symptoms:
- Dry, rough skin.
- Cracked skin with oozing of sticky discharge.
- Eruptions oozing honey-like fluid.
Sulphur
Overview:
Sulphur is useful for spongiotic dermatitis with intense itching, burning, and redness of the skin. It is prescribed when there is aggravation from warmth and washing, and relief from cold applications.
Key Symptoms:
- Intense itching and burning.
- Redness of the skin.
- Aggravation from warmth and washing.
Rhus Toxicodendron
Overview:
Rhus Toxicodendron is indicated for spongiotic dermatitis with intense itching that worsens at night. The skin may be swollen, red, and covered with vesicles or blisters. It is also used when symptoms are aggravated by cold and wet weather.
Key Symptoms:
- Intense itching, worse at night.
- Swollen and red skin.
- Vesicles or blisters on the skin.
Arsenicum Album
Overview:
Arsenicum Album is prescribed for spongiotic dermatitis with burning, itching, and restlessness. The skin may be dry, scaly, and may have eruptions with a burning sensation. It is used when symptoms worsen at night and improve with warmth.
Key Symptoms:
- Burning and itching of the skin.
- Restlessness.
- Dry, scaly skin with eruptions.
Mezereum
Overview:
Mezereum is helpful for spongiotic dermatitis with thick crusty eruptions and intense itching. The skin may be raw, inflamed, and sensitive to touch. It is indicated when there is oozing of sticky or watery discharge from eruptions.
Key Symptoms:
- Thick crusty eruptions.
- Intense itching.
- Raw, inflamed skin sensitive to touch.
Petroleum
Overview:
Petroleum is useful for spongiotic dermatitis with dry, cracked skin that may ooze and bleed. It is indicated for skin issues worsened by cold weather and improved by warmth.
Key Symptoms:
- Dry, cracked skin.
- Skin that oozes and bleeds.
- Aggravation in cold weather and improvement with warmth.
Calendula Officinalis
Overview:
Calendula Officinalis is beneficial for spongiotic dermatitis with raw, inflamed skin and superficial wounds or cuts. It promotes healing and soothes irritated skin.
Key Symptoms:
- Raw, inflamed skin.
- Superficial wounds or cuts.
- Irritated and sensitive skin.
Hepar Sulphuris Calcareum
Overview:
Hepar Sulphuris Calcareum is indicated for spongiotic dermatitis with painful, infected skin that is sensitive to touch and cold. It helps in cases where skin issues worsen from exposure to cold air.
Key Symptoms:
- Painful and infected skin.
- Sensitivity to touch.
- Aggravation from exposure to cold air.
Antimonium Crudum
Overview:
Antimonium Crudum is prescribed for spongiotic dermatitis with thick, hard crusts and intense itching. It is used when the skin is sensitive to touch and aggravated by heat and cold bathing.
Key Symptoms:
- Thick, hard crusts on the skin.
- Intense itching.
- Skin sensitivity aggravated by heat and cold bathing.
Natrum Muriaticum
Overview:
Natrum Muriaticum is helpful for spongiotic dermatitis with dry, cracked skin, especially on the edges of the hairline or around the mouth. It is indicated when skin issues worsen from sun exposure and improve with sea bathing.
Key Symptoms:
- Dry, cracked skin.
- Skin issues around the edges of the hairline or mouth.
- Worsening from sun exposure and improvement with sea bathing.
FAQs about Spongiotic Dermatitis
What is spongiotic dermatitis?
Spongiotic dermatitis is a type of eczema characterized by inflammation and spongiosis (fluid accumulation) in the epidermis. It manifests as red, itchy, and inflamed skin patches.
What causes spongiotic dermatitis?
The exact cause can vary but often includes allergic reactions, irritants, and underlying conditions like atopic dermatitis. Environmental factors and genetics may also play a role.
What are the symptoms of spongiotic dermatitis?
Common symptoms include red, itchy skin, swelling, and sometimes oozing or crusting lesions. The affected areas can be painful and may become infected if scratched excessively.
How is spongiotic dermatitis diagnosed?
Diagnosis typically involves a clinical examination of the skin. A dermatologist may perform a skin biopsy to confirm the presence of spongiosis and rule out other skin conditions.
Can spongiotic dermatitis be cured?
While there is no definitive cure, symptoms can be managed effectively with treatment. This includes avoiding triggers, using topical corticosteroids, and moisturizing the skin regularly.
What treatments are available for spongiotic dermatitis?
Treatment options include topical corticosteroids, antihistamines to relieve itching, and emollients to maintain skin hydration. In severe cases, systemic medications or phototherapy may be recommended.
Are there any home remedies for spongiotic dermatitis?
Home remedies may include oatmeal baths, aloe vera gel, and coconut oil to soothe the skin. It is essential to avoid known triggers and maintain a consistent skincare routine.
Is spongiotic dermatitis contagious?
No, spongiotic dermatitis is not contagious. It cannot be spread from person to person through physical contact.
Can diet affect spongiotic dermatitis?
Certain foods may trigger or worsen symptoms in some individuals. Keeping a food diary to identify and avoid potential allergens can be helpful.
When should I see a doctor for spongiotic dermatitis?
You should see a doctor if the condition does not improve with over-the-counter treatments, if the symptoms are severe, or if there are signs of infection, such as increased redness, warmth, swelling, or pus.